Cultural Competency in Healthcare
Cultural competency in healthcare is an important skill for healthcare providers to have, but what does cultural competency consist of, and what are the practical outcomes of being culturally competent? Individual values, beliefs, and behaviors about health and well-being are shaped by various factors such as race, ethnicity, nationality, language, gender, socioeconomic status, physical and mental ability, sexual orientation, and occupation.
Share This Post
Cultural competency in healthcare is an important skill for healthcare providers to have, but what does cultural competency consist of, and what are the practical outcomes of being culturally competent? Individual values, beliefs, and behaviors about health and well-being are shaped by various factors such as race, ethnicity, nationality, language, gender, socioeconomic status, physical and mental ability, sexual orientation, and occupation. Cultural competence in healthcare is broadly defined as the ability of providers and organizations to understand and integrate these factors into the delivery and structure of the healthcare system. The goal is to provide the highest quality of care to every patient, regardless of age, race, ethnicity, cultural background, English proficiency or literacy. In order to increase the cultural competence of the healthcare delivery system, health professionals need to participate in ongoing cultural competency training. Important to note, however, is that cultural competence is a process rather than an ultimate goal and is often developed in stages by building upon previous knowledge and experience. Therefore, in addition to participating in ongoing training, healthcare professionals can benefit from taking intercultural competency assessments and having individual development plans.
The population at risk for chronic conditions will become more diverse.
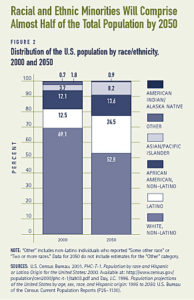
One dawning concern for healthcare providers are populations with chronic illnesses. They account for only 10% of the country, yet make up 70% of all hospital services. Older populations are most susceptible to chronic illness. In 2000, 35 million people — more than 12% of the total population — were 65 years or older. By 2050, it is expected that one in five Americans (20%) will be elderly. Moreover, this population will become increasingly diverse. By 2050, racial and ethnic minorities will comprise nearly 50% of the total population and 35% of the over 65 population. These numbers indicate that, as the population at risk of chronic conditions becomes increasingly diverse, more attention to linguistic and cultural barriers to care will be necessary. Of the more than 37 million adults in the U.S. who speak a language other than English, 18 million (48%) report that they speak English less than “very well.” Language and communication barriers can affect healthcare outcomes. For example, Spanish-speaking Latinos are less likely than Whites to visit a physician or mental health provider or receive preventive care, such as a mammography exam or influenza vaccination. Health service use may also be affected by the availability of interpreters. Among Limited English Proficient (LEP) speakers who needed an interpreter during a healthcare visit, less than half — 48% — report that they always or usually had one.
Language and communication barriers are problematic.
Language and communication problems may lead to patient dissatisfaction, poor comprehension and adherence, and lower quality of care. Spanish-speaking Latinos are less satisfied with the care they receive and more likely to report overall problems with healthcare than are English speakers. The type of interpretation services provided to patients is an important factor in the level of satisfaction as well. In a study comparing various methods of interpretation, patients who use professional interpreters are equally as satisfied with the overall healthcare visit as patients who use bilingual providers. Patients who use family members as interpreters or untrained bilingual staff, which can be nurses, clerks or technicians, are less satisfied with their visit.
Strategies for improving organizational cultural competence:
Some common strategies for improving the patient-provider interaction and institutionalizing changes in the healthcare system include:
1. Provide language access services such as interpretation and translation (not only during the clinical
encounter but at the appointment desk, on advice lines, and during medical billing)
2. Recruit and retain diverse staff that reflects the population being served
3. Implement organizational and individual cultural competence assessments
3. Provide ongoing training to increase cultural awareness, knowledge, and skills
4. Incorporate culture-specific attitudes and values into health promotion tools
5. Include family and community members in healthcare decision-making
For more information on how Spring Institute can help your organization become more culturally
competent, visit our Connecting Cultures in Health initiative at https://springinstitute.org/connecting-
cultures-in-health/
Read more Posts

The Transformational Power of Resistance
Are organizations that go through these motions but fall short of impactful follow-through demonstrating laziness or a lack of integrity?

Strategies for Mitigating Implicit Bias in the Legal Field
Unconscious bias can have a range of implications and potential consequences for legal professionals, including shaping interpersonal dynamics with prospective and current clients and colleagues and, in turn, influencing organizational dynamics at the smallest law practices and the largest firms alike.
